Optic Nerve Sheath Diameter (ONSD)
Tips & Tricks: in progress
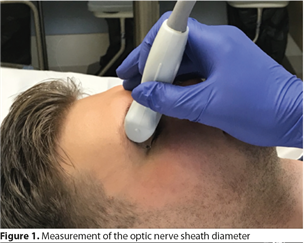
Image acquisition: a high frequency linear transducer is used (5-12 MHz). Smaller probes are preferred as these fit nicely into the orbit's cavity. The B-mode is used. The probe is positioned transversal and slightly above the eyelid (Figure 1; adapted from Neth J Crit Care March 2019;27(2): 81 - 6). Both eyes should be examined multiple times (optimal number remains unspecified). Measured are done with the patient in supine position, although the ONSD does not significantly change with patients's position. A barrier can be placed over the eyelid and avoid unnecessary pressure on the eye.
The optic disc is used as reference point and the optic nerve sheath diameter is measured at 3 mm behind the globe (Figure 2: adapted from Neth J Crit Care March 2019;27(2): 81 - 6). The optic nerve appears as a hypoechoic band. Slight rotation of the probe could also offer better visualization of the optic nerve.
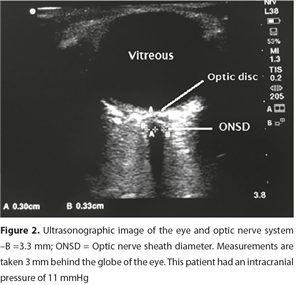
Image interpretation: In healthy adults, ultrasound measurements of the ONSD ranged from 3.7-5.4 mm. This is a relatively wide range. No relation has been found between ONSD and age, weight or height.
Most studies on patients were performed in emergency department (ED) or intensive care unit (ICU) patients. For qualitative assessment of a raised intracranial pressure (ICP >20 mmHg), a cut-off value of ONSD ranging from > 5-5.9 mm was found to have a pooled sensitivity of 90% and specificity of 85%. When compared to with findings of increased ICP on CT-imaging a cutoff value was found to have a sensitivity of 96% and specificity of 92%. For now ultrasound measurements can be used as qualitative measurement, as regarding ONSD measurement as quantitative measurement remains a matter of debate.
Reproducibility, feasibility and learning curve: Although only studied in a few studies, repeatability and reproducibility were found to be good. feasibility has not been studied in particular. Also, literature regarding the learning curve is limited. For less experienced operators around 25 scans are needed, whereas for more experienced operators 10 scan seems to be sufficient.
Limitations: Given te impact of increased ICP on patient outcome, nearly perfect accuracy of ONSD measurement is needed. Therefore, ultrasound measurements of ONSD should be used with caution.
Conclusion: Assessment of ONSD by ultrasound may serve as an additional diagnostic tool to diagnose a raised ICP. ONSD should not replace invasive ICP measurements of CT scans when indicated. Assessment of raised ICP should not be done by ONSD ultrasound alone, but always assessed in concert with available data from clinical examination and other diagnostic modalities
References:
N.S. Tjahjadi, W. van de Bergh, P.W.G. Elbers, D. Gommers, P.R. Tuinman. Point-of-care ultrasound of optic nerve sheath diameter to detect elevated intracranial pressure: Ultrasound in the eye of the beholder? Neth J Crit Care March 2019;27(2): 81 - 6
Ohle R, McIsaac SM, Woo MY, Perry JJ. Sonography of the Optic Nerve Sheath Diameter for Detection of Raised Intracranial Pressure Compared to Computed Tomography: A Systematic Review and Meta-analysis. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2015;34(7):1285-94.
Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive care medicine. 2011;37(7):1059-68.
Koziarz A, Sne N, Kegel F, Alhazzani W, Nath S, Badhiwala JH, et al. Optic nerve sheath diameter sonography for the diagnosis of increased intracranial pressure: a systematic review and meta-analysis protocol. BMJ Open. 2017;7(8):e016194.
Frumin E, Schlang J, Wiechmann W, Hata S, Rosen S, Anderson C, et al. Prospective analysis of single operator sonographic optic nerve sheath diameter measurement for diagnosis of elevated intracranial pressure. The western journal of emergency medicine. 2014;15(2):217-20.
Komut E, Kozaci N, Sonmez BM, Yilmaz F, Komut S, Yildirim ZN, et al. Bedside sonographic measurement of optic nerve sheath diameter as a predictor of intracranial pressure in ED. The American journal of emergency medicine. 2016;34(6):963-7.
Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocritical care. 2011;15(3):506-15.
Amini A, Kariman H, Arhami Dolatabadi A, Hatamabadi HR, Derakhshanfar H, Mansouri B, et al. Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. The American journal of emergency medicine. 2013;31(1):236-9.
Chief-editors
Pieter Roel Tuinman, MD, PhD, intensivist-epidemiologist
David van Westerloo, MD, PhD, intensivist
Editors:
Carlos Elzo Kraemer, MD, intensivist
Jorge Lopez Matta, MD, intensivist
Paul Wijnandts, MD, intensivist
Jasper Smit, MD, PhD student
Mark Haaksma, MD, PhD student
Micah Heldeweg, MD, PhD student
Annemijn Jonkman, technical physician, PhD student
Heder de Vries, MD, PhD student
Contact
Department of Intensive Care Medicine
Amsterdam University Medical Centres, Vrije Universiteit Amsterdam
Room ZH - 7D-166
De Boelelaan 1117
1081 HV Amsterdam, The Netherlands
prtuinman@hotmail.com
Department of Intensive Care Medicine
Leiden University Medical Center (LUMC)
