Ultrasound-guided PDT protocol:
The patient who has previously fasted for at least five hours is sedated and adequately positioned with hyperextension of
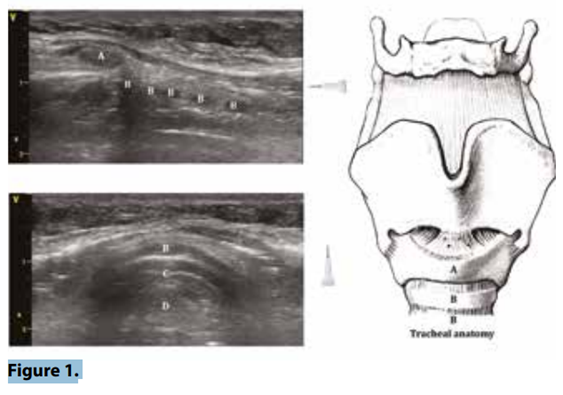
the neck. The ultrasound machine is placed at the opposite side of the operator. An ultrasound is performed of the neck in transversal and longitudinal view (figure 1). Cricoid cartilage and tracheal rings are identified, as well as pre-tracheal and para-tracheal regions of the neck searching for unexpected abnormal vasculature. A sterile field is prepared around the operation site and the
linear probe is used. The skin and subcutaneous tissue in the operation zone is infiltrated with local anaesthetics with adrenalin, which has
two functions. The first is vasoconstriction of subcutaneous capillaries/vessels and the second is increasing the resolution of
the neck landmarks by placing a depot of liquid which enhances the image quality beneath. At this point the endotracheal tube is retrieved to just above the vocal cords under visualisation with the use of the laryngoscope. This is only done if the patient has high ventilator support
parameters, arbitrarily a PEEP level >8 or high delta pressures. If ventilator parameters are low, which is almost always the case, we usually replace the endotracheal tube with a laryngeal mask since we feel that keeping the tube to facilitate the use of a bronchoscope is not necessary when using this ultrasoundguided technique. Having said that, bronchoscopy through a laryngeal mask is still feasible if needed.
The preferred tracheal ring space is chosen with the longitudinal ultrasonographic view (figure 1). As mentioned earlier this one is located anywhere between tracheal ring 1 and 4. The blue dilatator of the tracheostomy set is used to identify this localisation by pressing lightly on the skin and observing with the ultrasound at which tracheal ring level the pre-tracheal tissue is being pressed (figure 2A). This ‘mark’ is used as a guide and the linear probe is placed transversally at this level. (ref1)
Ultrasound guided percutaneous tracheostomy
The tracheal ring just beneath the tracheal ring space chosen is visualised. The midline of the desired tracheal puncture localisation is placed in the middle of the ultrasound screen, and the puncture needle (coupled to a 5 or 10 ml saline-filled syringe) is introduced perpendicularly to the skin and advanced until the needle is seen to pass the anterior tracheal wall with aspiration of air (figure 1B and C). Once this has been achieved, the ultrasound linear probe is discarded. At this point the needle is angled caudally, and is retrieved leaving the plastic catheter
behind. The guidewire is then introduced and once intraluminal placement is confirmed the plastic catheter is removed leaving the guidewire in the trachea (figure 2D). A small horizontal or vertical incision (depending if nearby vessels are observed) is made at each side of the guidewire to allow dilatation. The puncture site is sequentially dilated using the small dilator first followed by the bigger green dilator (figure 2E). Once introduced until the pre-specified marker on the dilator, it is left in situ for 1 minute as specified by its manufacturer (figure 2F).
The dilator is then removed leaving the guidewire behind. The trachea cannula is introduced using the guidewire and once in place the latter is removed and the inner cannula is introduced followed by connection to the ventilator. Correct placement is controlled by the presence of end tidal CO2 and/or with the use of the linear probe to confirm the presence of ‘lung-sliding’ bilaterally and/or a ‘seas shore sign’ on M mode
(figure 2G) which confirms bilateral ventilation. (ref1)

Reference:
1. To see or not to see: ultrasound-guided percutaneous tracheostomy. J.E. Lopez Matta, C.V. Elzo Kraemer, D.J. van Westerloo. Neth J Crit Care March 2018;26(2): 66 - 9 (https://njcc.nl/sites/nvic.nl/files/pdf/original-article_12.pdf)
Chief-editors
Pieter Roel Tuinman, MD, PhD, intensivist-epidemiologist
David van Westerloo, MD, PhD, intensivist
Editors:
Carlos Elzo Kraemer, MD, intensivist
Jorge Lopez Matta, MD, intensivist
Paul Wijnandts, MD, intensivist
Jasper Smit, MD, PhD student
Mark Haaksma, MD, PhD student
Micah Heldeweg, MD, PhD student
Annemijn Jonkman, technical physician, PhD student
Heder de Vries, MD, PhD student
Contact
Department of Intensive Care Medicine
Amsterdam University Medical Centres, Vrije Universiteit Amsterdam
Room ZH - 7D-166
De Boelelaan 1117
1081 HV Amsterdam, The Netherlands
prtuinman@hotmail.com
Department of Intensive Care Medicine
Leiden University Medical Center (LUMC)
